This post was inspired by people at Twitter – so thank you for all of the support in gathering the resources for this! One of the things that I want to do on this blog is look at ways to increase access to healthcare. I’ve talked about the health inequalities that exist, and there are probably a lot of different reasons why these exist. There may be biological predispositions that we don’t understand yet (however, this is being researched into). There is likely a large psychological element at play (especially in people falling into the ‘high functioning’ bracket). But ultimately the largest element at play is likely the social one.
Whether we like it or not, the ability to interact with others and form a connection is incredibly important to survival on this planet. You need to be able to find your people and make your tribe in order to have support, otherwise you risk being caught out by yourself and feeling that isolation. While autistic people having difficulties with socialising, the majority of people still crave it – craving something that you find difficult to do is painful. Therefore, the effects from this are likely a large contributor.
I don’t have the answers on how to solve this. That is beyond my abilities at this second. But what I can do is focus on what I do have the experience from. What I have seen when accessing health care services is that autism is not understood (even to the most minute detail in some cases). The health care profession does not have the systems in place to help autistic people. This is apparent by the fact that an autistic person can walk into an accident and emergency department, one of the worst places for sensory overload that I have ever experienced, and there is no consideration about what would make them more comfortable there. This then continues when looking at wards where no thought is put in.
The staff working there seem to have two reactions to it: they either ignore it (as the person is not causing them any difficulties right now), or they think that the person is weird and they are a task they need to work around in order to complete their job (because they are causing them difficulties). This may not be true in all cases, but from my experience I haven’t seen much good practice. I’ve seen doctors not communicating to non-verbal people when that person is clearly communicating to them. I’ve seen doctors be informed about a person’s sensory difficulties and then not consider changing the current environment at all. I’ve seen staff think about stereotypes instead of learning about the individual. How our healthcare system is currently is not set up properly for autistic people.
To an extent, that’s not their fault. For England, the NHS is stretched incredibly thin and all of the staff are working their very best to keep it running at the moment. I can understand a minority group being forgotten in that system where they are trying to keep it going to protect the majority of people. Additionally, at least they are not letting people die from countless conditions they can do something about. However, in this way the NHS is self-defeating as it is currently so focussed on the current day that it ignores the future implications. Not talking to a worried patient today could mean that they go to their GP five or six times and feels frustrated, wasting time and money where a quick but clear explanation could have saved this.
In regards to autism – whenever an autistic person has a bad experience going into hospital (which, quite frankly, can be a traumatic experience if no one understands what is important to you) then they are not going to want to go back. If they don’t go back, they may not have the right tests at the right time. This means that no one notices that they have had a change in their bowel habit and develop bowel cancer until it is too late to treat it completely. Then they die. This is an extreme example, but is a likely one. From my experience, autistic people are worried about seeing their doctor as they feel they will not understand.
I want there to be a ways to help autistic people access healthcare and make it so that it doesn’t have to be so traumatic in the present, making it easier to see doctors in the future. To this end, it may mean that we pick up health problems earlier and so can avoid worse outcomes.
To this end, today we are going to look at hospital passports. These are documents that you can produce ahead of going to your doctor in order to communicate what you find challenging and what it is important for them to know. Thanks to people at Twitter (@AspieHuman, @carolinehearst, @D0V0S0 – thank you!) I have learnt about two methods that exist. I have taken these and completed one of both for myself, and one of both for Darni (they kindly agreed to help). From this I can ultimately say that both tools are helpful, but there are some places where they would be more effective. I’m going to take you through the tools showing you examples from Darni’s profiles and discuss some of this.

Type 1 – AASPIRE (Academic Autistic Spectrum Partnership in Research and Education) – Autism Healthcare Accommodations Report
(Link: https://www.autismandhealth.org/?p=ahat&theme=ltlc&size=small)
This is a handy toolkit made by a group based at Portland State University in Oregon, United States. It produces a report that looks like this:
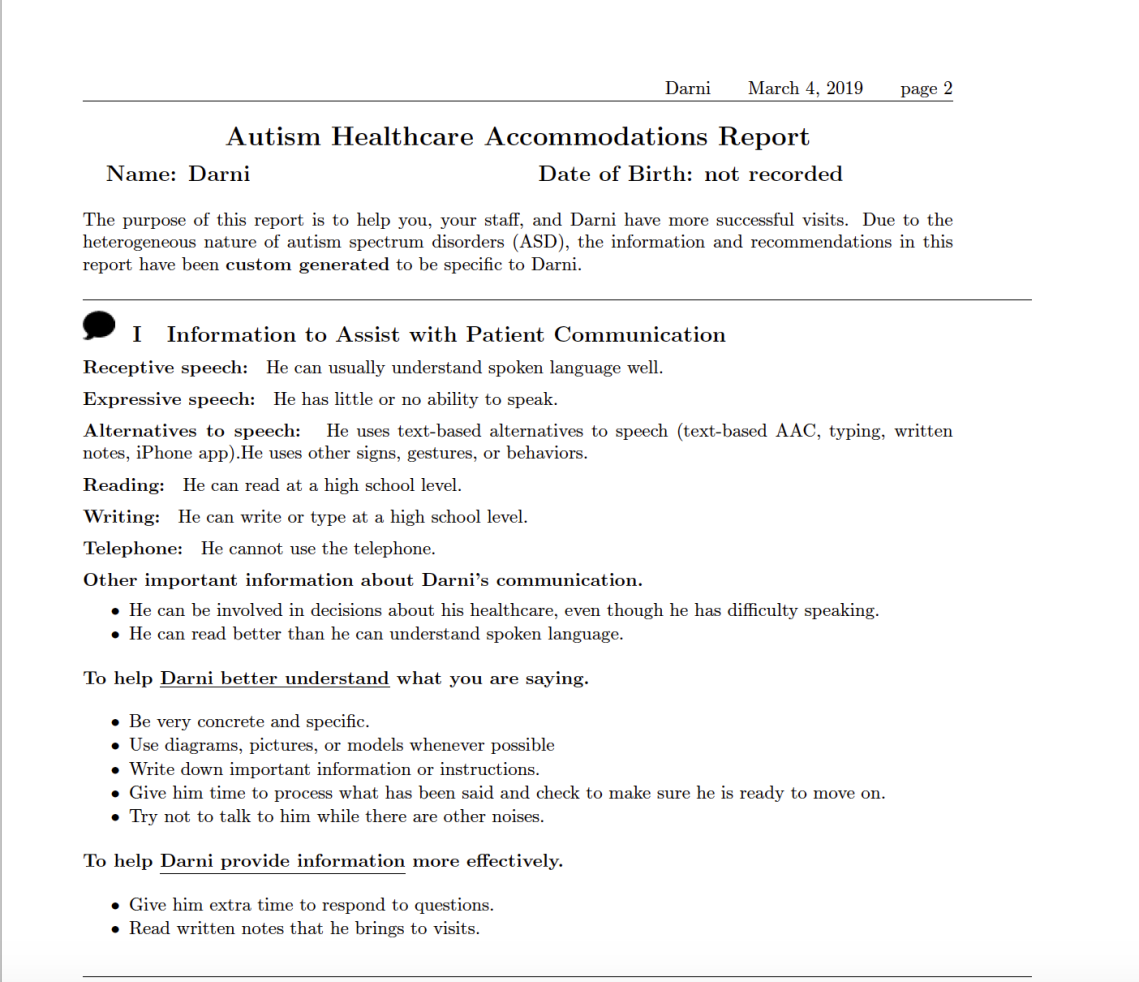
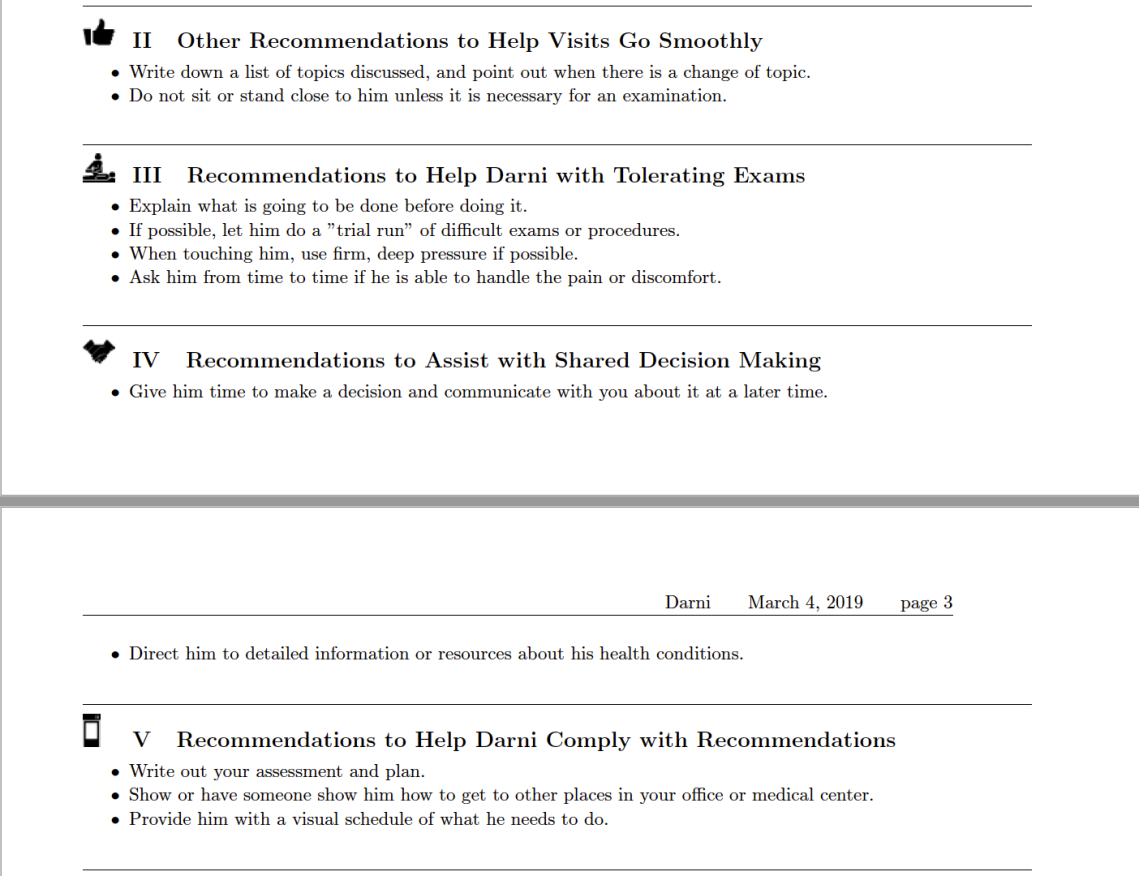
My first impression of this is that it is aimed towards the US health system, so is not completely applicable to the UK. This is a bit of a con for me. However, on looking through it I found that this could be a helpful tool for use in primary care in the UK. The website links to a toolkit webpage with fields to complete. The toolkit is adaptable to provide larger font sizes, a different colour background and read aloud text, which is great. What it does it goes through the challenges someone has, their skills, what is important to them, and what healthcare professionals can do to help. It has multiple ways of being adapted to the individual.
When I completed this for Darni, the first question was about whether I was completing the tool for myself, someone who is not me but is male or someone who is not me but is female. This was a little bit of an unfortunate start as Darni is non-binary. However, on completing the form for myself later, if completing it for yourself they later ask your gender and give an option for non-binary identity.
It then asked about the methods that they can communicate in, including whether they can use the telephone (helpful to know for anyone trying to organise appointments). One of the most helpful things about this tool is the number of suggestions they give you of how to help. While they note that you shouldn’t exceed a certain number (which is just good practice anyway, the more you put in the less likely you are going to get any) they provide a lot of possible choices. This was great when thinking about ways to help and felt really empowering to me that you could ask for all of these things. We went through and picked out a load of ways to help with Darni’s communication (using pictures to help, writing down important information, giving them more time to process and respond to questions, being concrete and specific, reading notes that they bring to the visit).
It then asked about things to help before, during and after the visit. This followed the same formula of providing lots of suggestions, which was great. After this it asked questions about Darni, trying to get to know them better. In my opinion, this would have been helpful to do at the start rather than midway through as it helps to frame the report in a positive manner, but that’s just my feeling. The section goes through the positives (what they are good at, what their special interests are) and then goes through what can make them anxious, how they would communicate that and how you can help to prevent a meltdown.


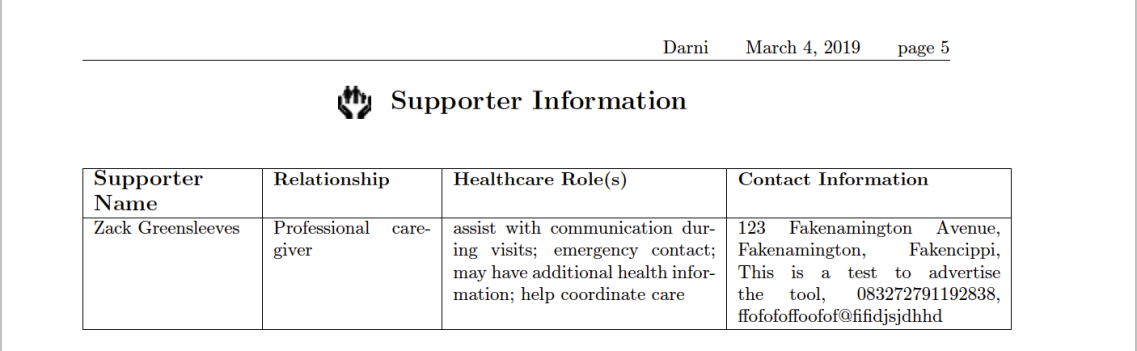
These are all pretty standard things, but the form does it in a good way. Finally, it asks about anyone who supports them. This includes people who are their guardian or people who have lasting power of attorney. However, it also includes personal assistants (of which I am Darni’s), family members and partners. It then leads onto asking a few more questions to finish up, and discussing whether you would need help to schedule appointments and organise transport (for which they add on a little bit of extra information onto the document.
The webpage then generates a pdf document using all of the information inputted, which you can then copy and provide to a healthcare professional of your choosing as appropriate.
Overall, I really liked this tool. It gave me a lot to think about and lots of suggestions for improving how I could access healthcare. In the end, the golden rule with healthcare is that you just need to ask. You may not get everything you ask for, but if you don’t ask then you definitely won’t. If you ask then you may get something, and so it’s worth trying things like this. This tool is limited for use outside of the US and I imagine it would have the potential to be ignored by healthcare professionals. But it is worth a try. Also, if more people do it then health care professionals will get more used to it and may become more receptive to it, which would be nice.

Type 2 – National Autistic Society – My Hospital Passport (for autistic people)
(Link: https://www.autism.org.uk/about/health/hospital-passport.aspx)
This is a second tool made by the National Autistic Society. This is great for people in the UK as it is more applicable to the country, but I imagine this one would be helpful for a lot of places (resembling a standard one page profile, but over more pages). This passport is a clear way of putting information succinctly for healthcare professionals who haven’t met you before.

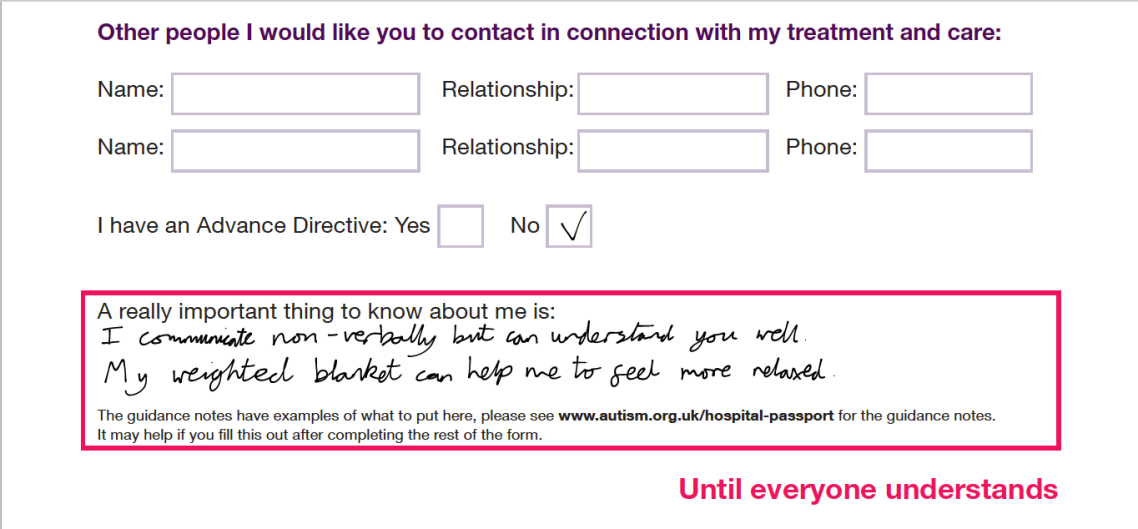

From the stance of ‘clerking’ in patients (talking to a patient, understanding why they are here and getting information about their background) this is a really helpful tool for the healthcare professional. This provides a person’s medication, allergy and past medical history. This is great as the doctor then doesn’t need to ask as many questions, making everyone happy. It also gives the names and details of other people important to you and so allows the doctors to contact them if they need more information.
An important note with this tool is that you should complete it after looking at the hospital passport guidance document. Without this you can miss a lot of the information that should be put into each section, so it’s important to refer to this. I completed each section while looking at this document, which I think was helpful.
This tool has a bit of a flaw compared to the other one in that you need to complete it by writing on it. Unless you have a pdf editor of some variety, there are not fields you can fill out so you need to write onto it with pen (or other ways, I used my tablet with some writing software). For me (who doesn’t have the greatest handwriting), it makes it a bit messy. What would be really helpful was if they adapted it so you can fill out the fields on the pdf document, and I would suggest that as a way they could improve the form.
It provides a place to state the one or two sentences of information that will make everyone’s life easier (in what is important to you). If you want people to not touch you without you knowing, put it down there. If you have a specific way of communicating, put it down there. If there is something crucially important to you, then it can be put on the front page. Then, if someone gets this given to them, this is one of the first bits of information they will see. This is really helpful for you to communicate what is really important to you.
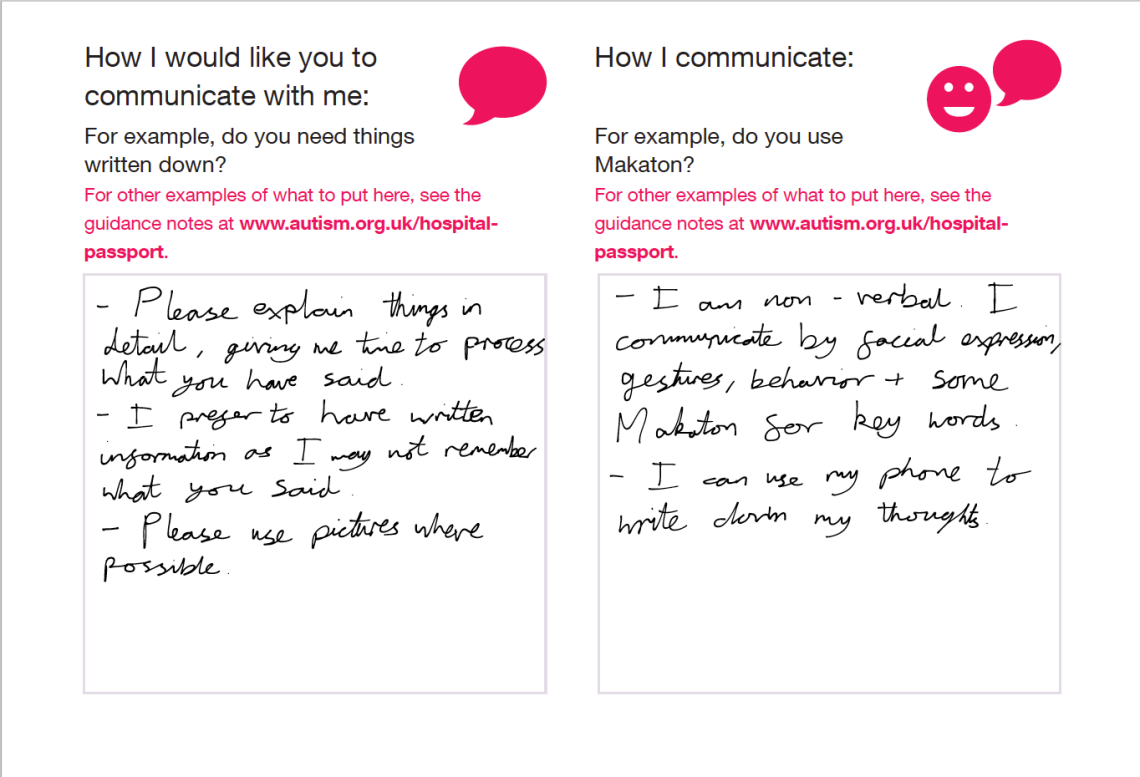
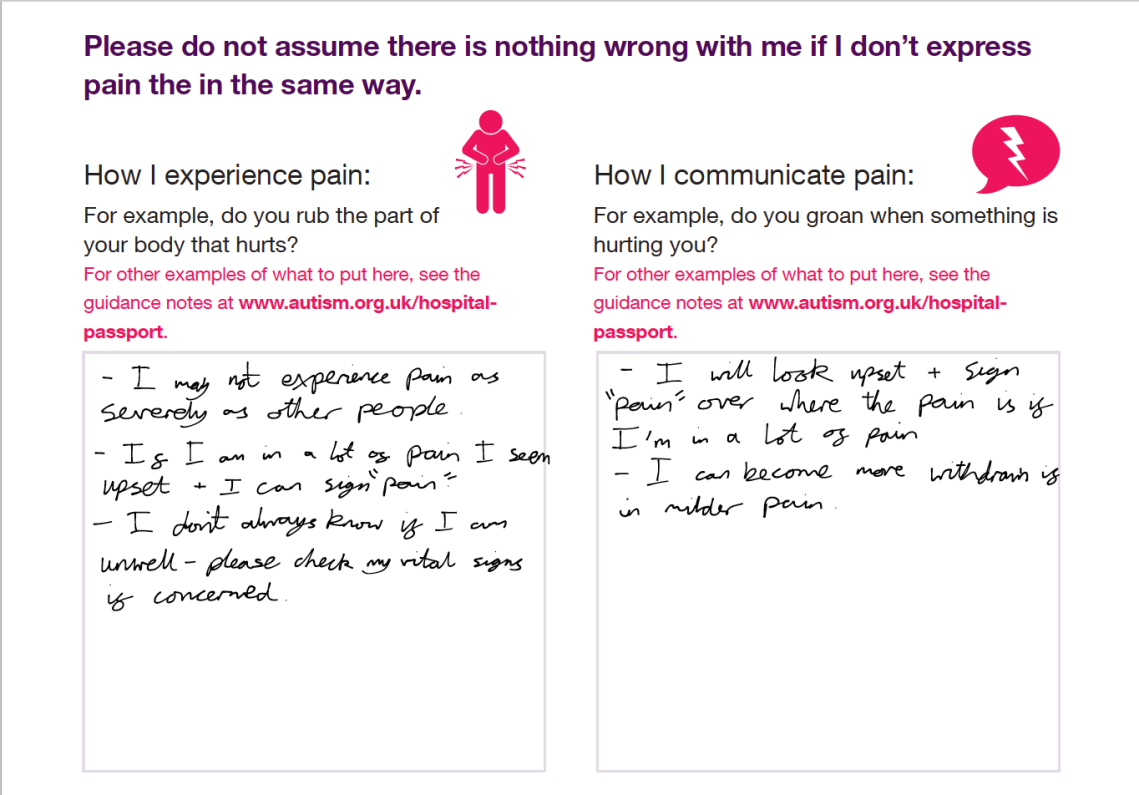
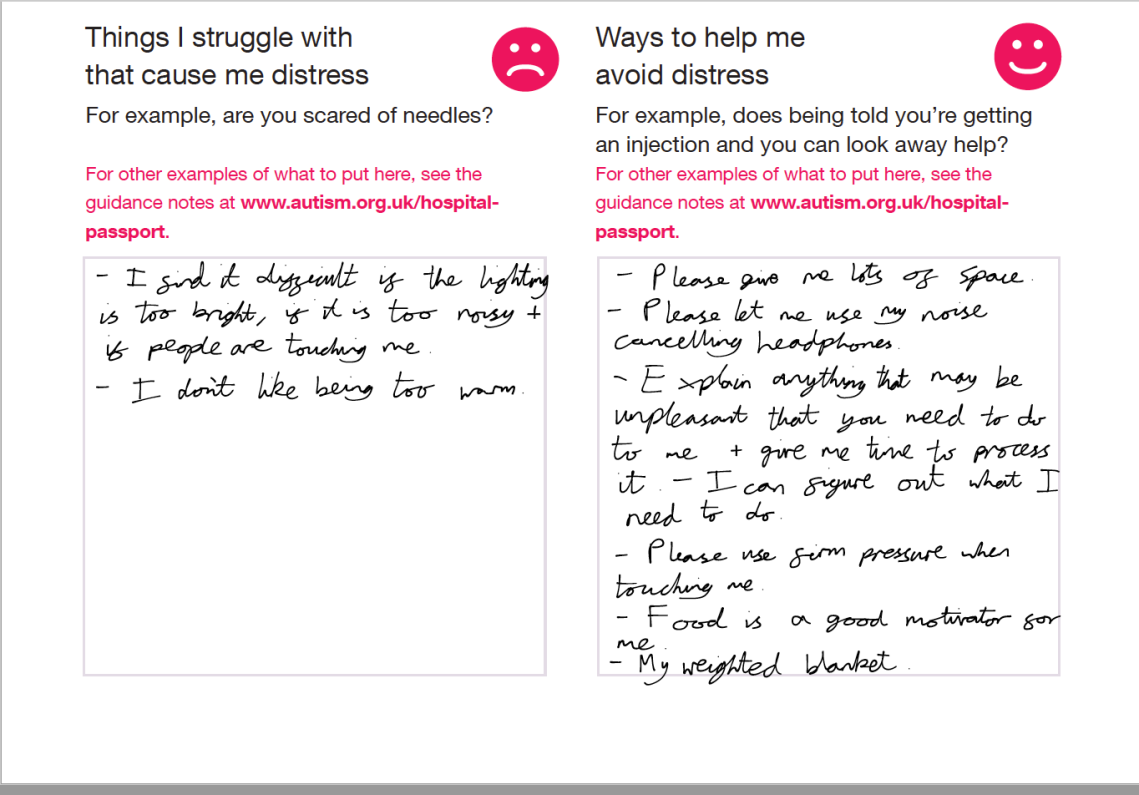
After going through all these bits it looks at communication (similarly to the other tool). It doesn’t give much space, which is good as then people are more likely to read it if they are busy. It then talks about pain, which is really good. Autistic people can experience pain differently, and so discussing this is really important. Again, this aids with the communication section. After this is talks about things that cause distress and ways to avoid it. What I was really impressed about with this tool is that this section is extremely practical towards certain healthcare procedures. It looks for things that can be done to help and it really means it. Are you afraid of needles? Are imaging tests going to be a problem? They have specific ways to help with these. This was really nifty.


It then does a similar thing to the other tool of looking at the positives – what are your sensory needs, what are your special interests, what makes you happen and what other things you should know about me. This is really good and helps to frame things. Both tools put this section later on. However, on thinking about this it means that people who are trying to read it quickly see the important bits for helping your immediately, but they can find out the rest if they look a bit further.
Finally, the form has a section on mental capacity to state that just because you are autistic, this doesn’t necessarily affect your mental capacity. I have a slight issue with this as the first sentence is a bit poorly written having a double negative in it, which confused me while I was reading it at first (“Please do not assume that I don’t have mental capacity”). Therefore, I scribbled out the “do not” and “don’t” on my form. Again, if I was to improve this form I would change the wording of that, but otherwise this is important to state.
What I would say with this form is that it is really helpful for accessing hospital services and, if I was to complete just one form, I would do this one. However, the AASPIRE tool is really good for getting you to think about the adaptations that would be helpful and, in my opinion, is probably more helpful for accessing GP services where they have more time to get to know you and can help you in a greater variety of methods.
Conclusion
Overall, these tools are really helpful for helping people to access hospital if the hospital staff will look at them. I would love to see this being used more widely across healthcare, as I feel this is really important and would save everyone a lot of time. However, I feel that healthcare staff would probably not have the awareness of these profiles and so not be used to using them.
Therefore, I have a few suggestions about how to use these to their best potential:
- Make about six copies – This is an arbitrary number, but you need at least four: one for the nurses, one for the doctors, one for your bedside notes, and one that you keep around for copying for if anyone else needs them. Given that you may need to see other therapists, it may be better to have more than three so I suggest six to be safe.
- If going by accident and emergency – Give a copy to the triage nurse (the first nurse who will see you) and to the doctor who will see you first (the clerking doctor). Tell them that you have autism, this is a document that will help you to access the service better and provides a load of information that can help them to know you better, including your medical history (the last part is important for making sure that they read it).
- When you get to a ward – Check if a copy is in the notes (if possible ask that it can be put at the front of the notes so that anyone will read them the moment that they pick up your notes). Ask for a copy to be put in your bedside notes (ex. Observation charts). Basically make sure the information is accessible.
- Then talk to the nurses about it. Nurses are great and are the people most likely to read these notes and get to understand you. Hopefully they will then discuss it with the doctors when they are doing their ward rounds and in this way it provides more information to all the professionals.
- If a new specialist/therapist comes to see you (who may not have read your notes), you can provide them with a copy of the profile for them to read.
In this way, you are more likely to have people read the document. At that point it is up to them to support you properly (though sadly you may need to either advocate more for yourself, or get someone else to help you in order to get this to happen. But we’ll look into ways to assist with that in the future).
These are really helpful tools, but depend on healthcare staff reading them. Therefore, we need to motivate people to do this. I hope that healthcare professionals will read this and spread the message out there about these documents and how they can be important. Overall, thinking in that long term, if people can work within a system like this then I believe that autistic people will have better experiences in healthcare and will feel more comfortable accessing services. Through this there is a chance of extending people’s lives, which is really worthwhile.
Thanks for reading! Please let me know if you have anything in regards to healthcare access that you want me to cover. This is really important to me and so if you have any suggestions for what you want me to talk about or look into then please let me know.

References:
AASPIRE – Autism Healthcare Accommodations Tool (https://www.autismandhealth.org/?p=ahat&theme=ltlc&size=small) Last accessed: 7th March 2019.
The National Autistic Society – My Health Passport for autistic people tool (https://www.autism.org.uk/about/health/hospital-passport.aspx) Last accessed: 7th March 2019.



1 Comments